Past Programs at One Mind: ASPIRe
ASPIRe (Accelerating Serious Psychiatric Illness Recovery) is One Mind’s initiative to support those with Serious Psychiatric Illness (SPI). ASPIRe aims to provide gold-standard, individualized care that has been shown to dramatically improve outcomes.
About ASPIRe
Serious Psychiatric Illness is a major unmet health need. Often referred to as serious mental illness, SPIs include schizophrenia, bipolar disorder, major depressive disorder, and other psychiatric conditions that substantially interfere with major life activities. The impact on the individual and on society is especially large because 75% emerge in youth between the ages of 10 and 24 years. Ultimately, 7.5% of youth between the ages of 18 – 25 years and 20% of adults are affected.
There are no cures for SPI, but it can be effectively managed with pharmacological and psychosocial interventions. The rates of remission and recovery are difficult to capture, but the best estimates suggest recovery rates of approximately 25% for bipolar disorder and schizophrenia and 65% for major depressive disorder. A large nationwide survey conducted in 2014 and 2015 also found that 70% of individuals in the USA did not receive any care. We can and must do better.
Similar to most diseases, prevention and early intervention are key to better outcomes, which is what the One Mind Accelerating Serious Psychiatric Illness Recovery (ASPIRe) initiative aims to achieve.
Goals
- 100% access to effective, personalized care for individuals at risk for or living with serious psychiatric illness by 2040
- 75% recovery rate for individuals with serious psychiatric illness by 2040
Healing the lives of those with SPI
Many genetic, environmental and social factors play a role in the development and progression of serious psychiatric illness, and no single organization can address them all. Advances in care require multiple stakeholders, but they often work in silos. The result is that translating knowledge from research into something useful for people often takes years or even decades.
To accelerate the process, the ASPIRe initiative is developing a patient-centered model that starts with this question: What is needed to change the trajectory for individuals with serious psychiatric illness from one of despair and disability to one of hope and recovery?
We identified 5 essential needs: access to knowledge, early detection and intervention, access to effective care, better diagnostics and treatments, and implementation and evaluation in real world settings.

Roadmap to Recovery
Access to Knowledge
One Mind is raising public awareness and reducing stigma about mental health through large scale education.To raise public awareness and reduce stigma surrounding psychosis, One Mind is supporting a separate division, One Mind All Media, to enable large scale education using a variety of platforms. Examples include Brain Waves, a weekly webcast interview series with scientists and people with lived experience, a Scientific Symposium at the One Mind Music Festival, and sponsorship of the nationally focused Well Beings public media campaign that includes a PBS film on youth mental health and stigma produced by Ken Burns, set to air nationwide in early 2022. This will be the first of three Ken Burns films over the next 10 years.
Early Detection & Intervention
One Mind is facilitating mental health screening and access to digital resources for youth experiencing or at risk for psychosis.
The shorter the duration of untreated psychosis, the better the outcomes. One strategy to minimize the duration of untreated psychosis is to work with primary care providers and schools to enable large scale mental health screening. To address the challenges of achieving this goal, One Mind created a think tank on “Youth Mental Health Screening and Referral” to offer guidance on what is currently in practice and develop a strategy for scaling up nationwide.
In addition, the One Mind Strong 365 program is developing a platform for digital outreach that connects individuals seeking information about psychosis online with referral to high quality treatment centers and other resources.
Access to Affective Care
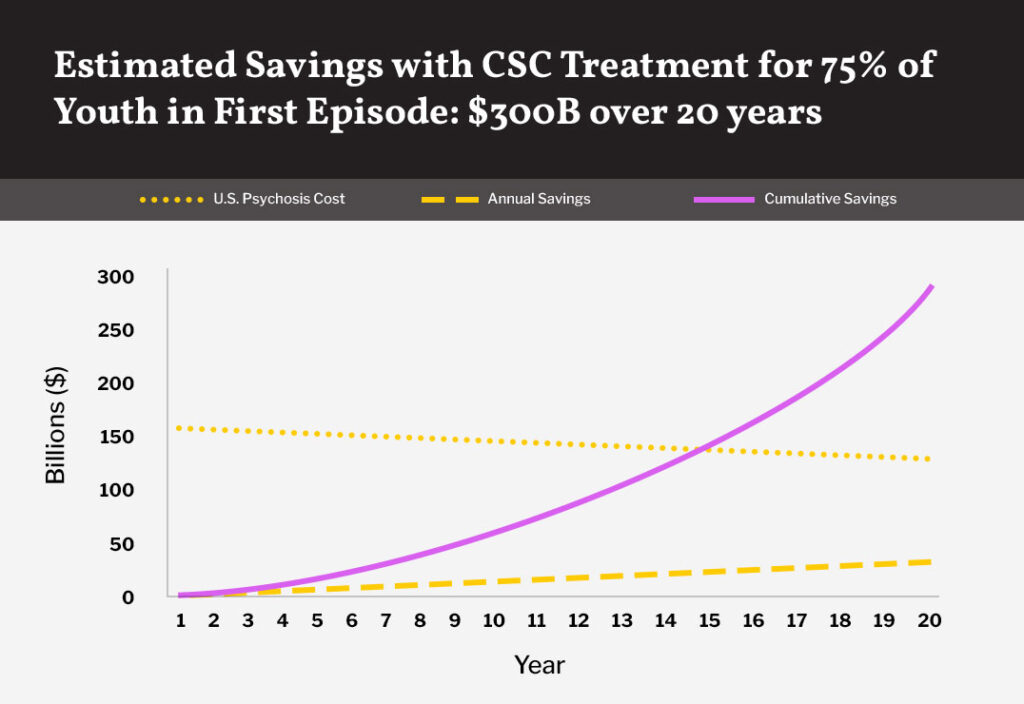
Bolstering the capacity of clinics that provide Coordinated Specialty Care (CSC), the gold standard for psychosis treatment, is critical for patients’ recovery.
A shortage of trained personnel and facilities is another major impediment to accessing coordinated specialty care (CSC), considered the “gold standard” for psychosis treatment. CSC is a recovery-oriented treatment program that leverages a team of specialists who work with the patient to create a personal treatment plan. We estimate that the current capacity of clinics providing CSC is less than 20% of what is needed.
To address the lack of capacity, we launched the Elizabeth Morgan Brown Center, a new One Mind ASPIRe clinic in Sonoma County in partnership with Kaiser Permanente Northern California Community Benefit Program. Lessons learned about the feasibility and utility of creating this CSC clinic will be applied to the development of future clinics.
Affordability is another critical barrier to access. Ironically, individuals with private insurance are often most vulnerable because of the lack of billing codes for insurance providers. One Mind is advising Kaiser Permanente and the California Mental Health Services Oversight and Accountability Commission on their partnership to investigate the feasibility and cost-effectiveness of private insurance reimbursement for CSC for psychosis. These efforts will inform and facilitate reimbursement policies by private insurers nationwide for psychosis as well as for other SPIs.
Better Diagnostics & Treatment
Developing biomarkers for mental health and neurological disorders will shorten the time needed to make a diagnosis, and increase accuracy.
Diagnosis is currently reliant on symptoms, which is problematic because there is a large overlap in symptoms across mental health and neurological disorders. This issue can prolong or even prevent an accurate diagnosis. Diagnostic tools that are based on biological indicators (biomarkers) will shorten and increase the accuracy of diagnosis. In addition, biomarkers will enable the development of more targeted therapies with fewer unwanted side effects.
The development of biomarkers is one of the major objectives of the Accelerating Medicines Partnership – Schizophrenia (AMP-SCZ), which is coordinated by the Foundation for NIH and includes industry and non-profit organizations, such as One Mind, as well as research organizations, regulatory agencies, and advocacy groups.
Implementation and Evaluation in Real World Settings
One Mind is supporting networks for Coordinated Specialty Care (CSC) providers to collaborate and learn from each other to improve performance and patient recovery.
Coordinated specialty care is currently the gold standard treatment for psychosis, but much remains unknown about which aspects of the care are most effective and for whom. It is now ready for wider adoption in real world environments and implementation research to evaluate and improve upon its performance.
In collaboration with the State of California Mental Health Research and Oversight Commission, One Mind is supporting EPI-CAL, a learning health care network for community-based providers among six counties in California. This is expected to expand to more counties in the future. EPI-CAL has also been selected to join a larger, NIH-funded network called EPINET, providing opportunities for collaboration on a nationwide scale. Strategies for learning healthcare networks that emerge from EPI-CAL can also be applied to other serious psychiatric illnesses in the future.
Partners
ASPIRe’s projects are a collaborative effort between a wide range of organizations working to support those with SPI, including: The Foundation for the National Institutes of Health (FNIH), Elizabeth Morgan Brown Memorial Fund, Strong 365, Kaiser Permanente, and Well Beings.